Proper and thoughtful preparation before physically demanding tasks is always advisable but exercising under heat stress sets further considerations for athletes and fitness enthusiasts as heat has a major negative impact on endurance performance which can be attenuated with heat acclimation. The benefits of heat acclimation are not restricted to the athletic population but are also present in soldiers carrying out missions in extreme heat, occupational populations that must perform work-related tasks in hot environments, clinical populations that are prone to heat-related health hazards, and anyone expecting to be exposed to heat in the near future.1
Understanding human heat balance, defined as the interaction between heat gain and heat loss, may improve heat acclimation strategies. Heat balance is regulated by factors such as humidity, air velocity, and solar radiation. With increased relative humidity, heat loss through evaporation, or sweating, is decreased, while high solar radiation increases heat gain. Air velocity, affected by wind and movement speed, may lead to either heat loss or gain depending on the thermal gradient between the skin and the surrounding air. Importantly, task-dependent and personal parameters such as intensity and duration of exercise, wearing of protective equipment or clothing, age, body mass, sex, morphology, and aerobic fitness further impact heat balance.1 While understanding the multifaceted factors influencing heat gain and loss provides useful insight on how to influence heat balance, understanding how heat balance affects physical performance and heat acclimation can prove to be equally important.
Heat Acclimation
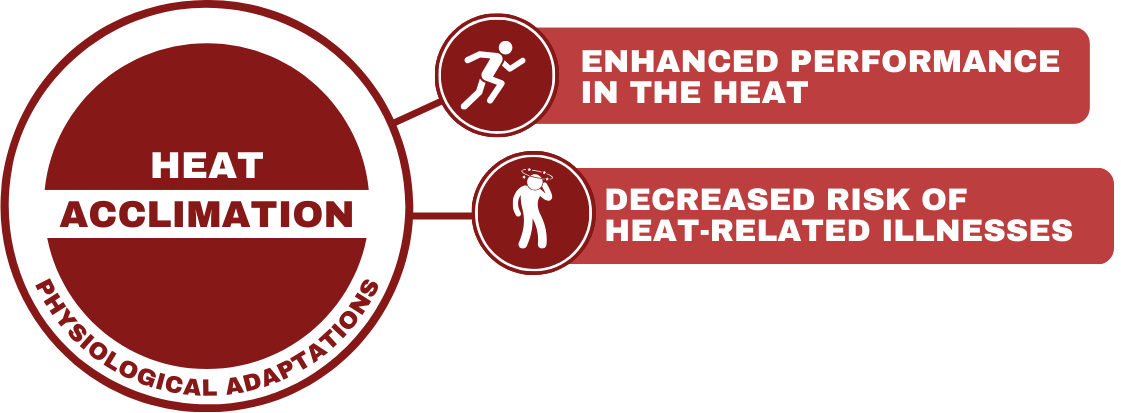
Heat stress intensifies many physiological responses that occur during intense and prolonged exercise. In practice, heat stress can reduce time to exhaustion during constant rate work exercise and decrease work rate in self-paced exercise. The negative impact of heat is mediated by adjustments in cardiovascular, central nervous system, and skeletal muscle functions. These adverse changes can be mitigated through repeated and/or prolonged exposure, as it triggers physiological adaptations that enhance heat tolerance and physical performance in hot conditions. Moreover, such exposure helps reduce heat-related health risks.1
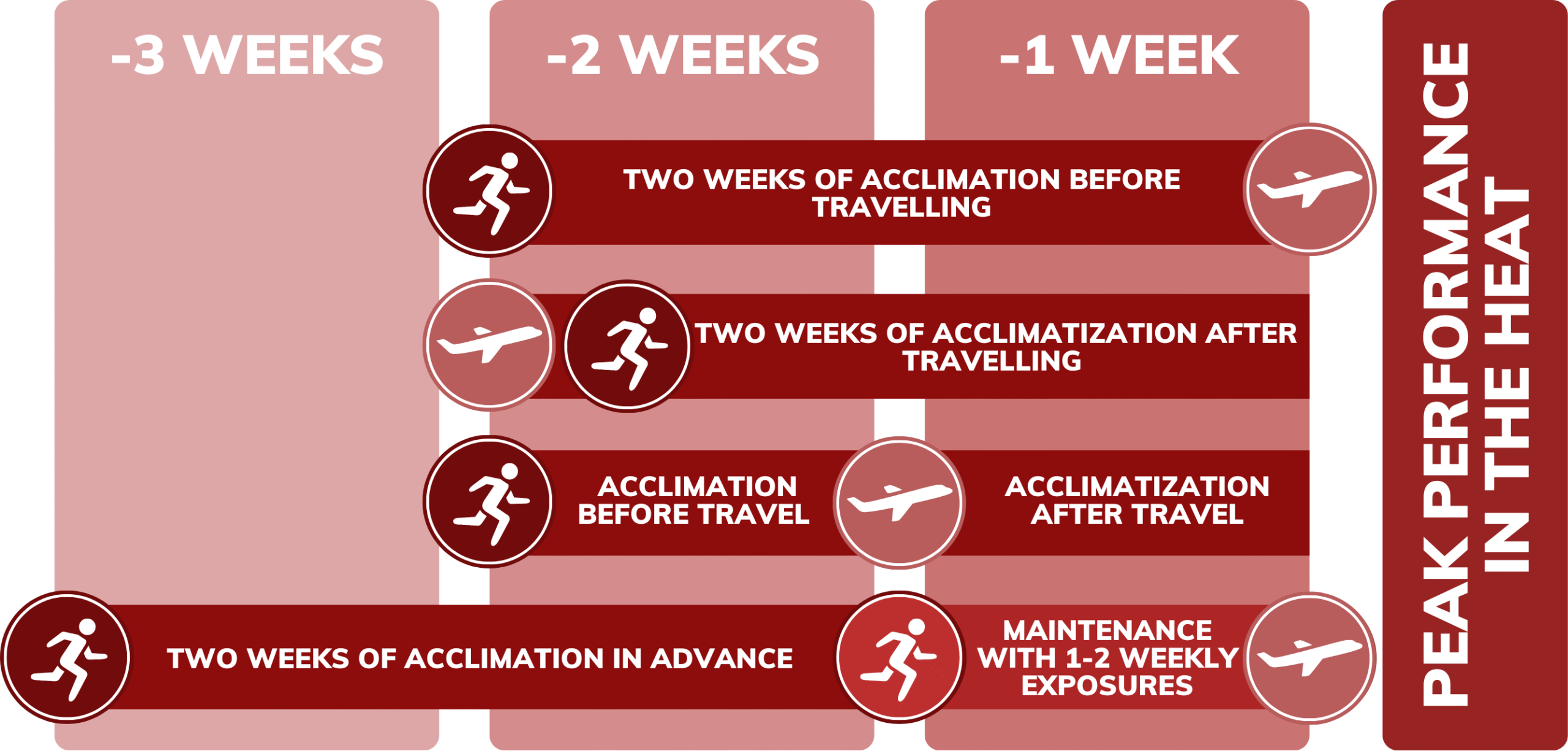
Heat acclimation begins rapidly upon exposure and significant benefits are acquired during the first week of the acclimation period, including a lower heart rate during submaximal exercise and a lower core temperature. Individuals wanting to maximize the available benefits should still aim for approximately two weeks of daily exposure as some physiological adaptations, such as improved sweat rate, require a longer time to develop.1 If necessary, the acclimation period can be interrupted by days of no-exposure, but this in turn slows down the acclimation process requiring a longer acclimation period if more than 1—3 heat exposures are missed.3
Heat Acclimation Protocols
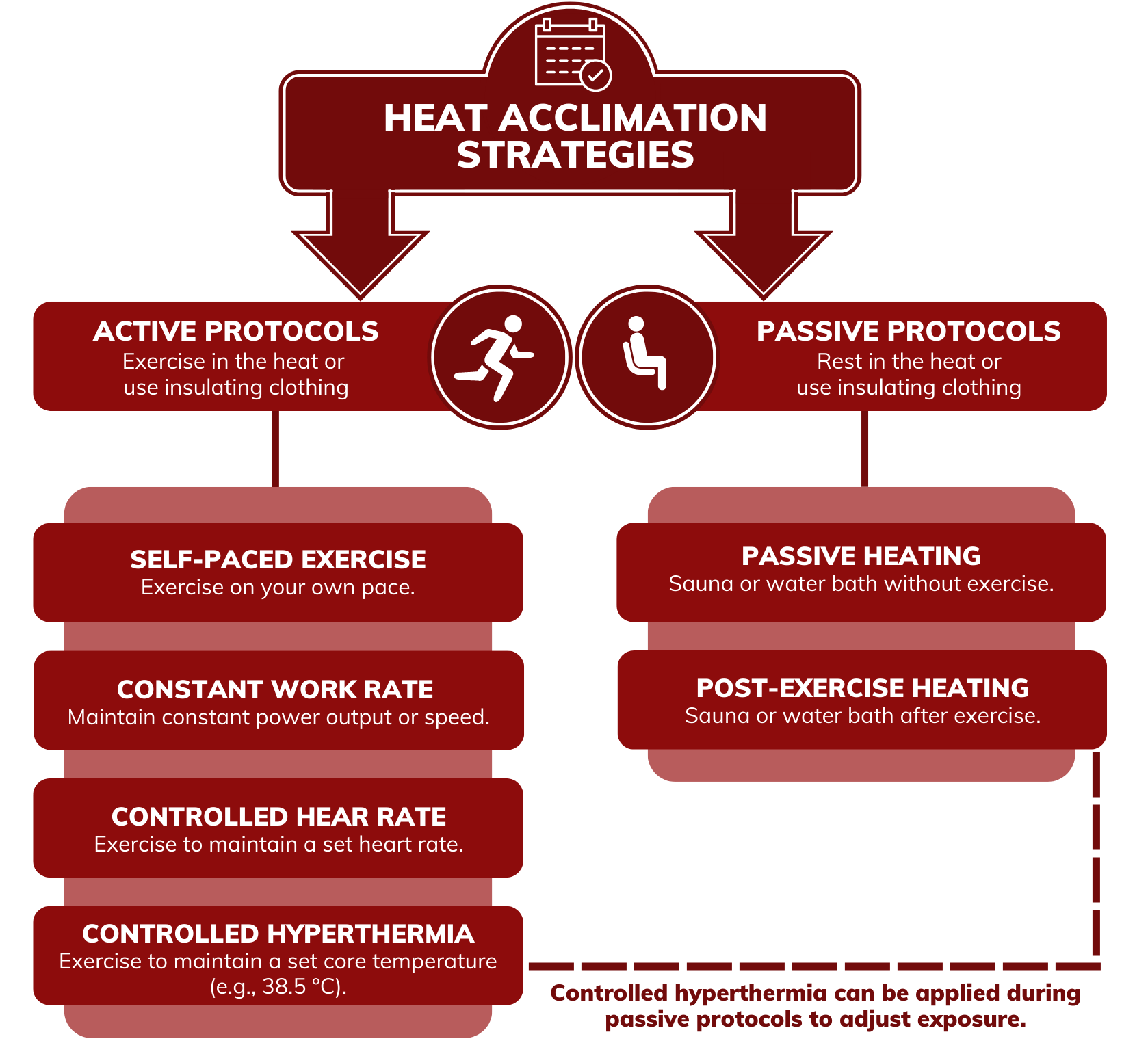
There are numerous ways to acclimate and to acclimatize to heat. Acclimation usually refers to the artificial adjustment of one or more environmental factors (i.e., temperature, relative humidity) to facilitate adaptation, while acclimatization refers to the adaptation gained from exposure to a natural environment. While a clear difference exists between the two conditions, they are often used interchangeably and can provide similar benefits to physical performance, health, and thermal comfort. There are two main heating strategies to implement when acclimating to heat: active and passive. Active heating strategies refer to the combined use of increased thermal exposure and exercise, while passive strategies rely solely on increasing thermal exposure.1 If increasing thermal exposure via increased temperature is not possible, using additional clothing can be considered as an effective substitute.5
Active heating strategies use the combined effects of increased heat stress and exercise but the best way to control the intensity of exercise is debated. Researchers, coaches, athletes, and military personnel have used self-paced exercise, constant work rate exercise, controlled hyperthermia (exercise is adjusted to maintain a set core temperature between 38.5 to 39°C), and controlled heart rate exercise (i.e., maintain heart rate at 65% of maximum) to elicit heat adaptations. While each of these strategies have their benefits and drawbacks, it is important to provide a constant thermal impulse for adaptations to occur. Hence it is recommended to adjust the acclimation protocol as progress is made. When the body adapts to better tolerate the hot environment, it is possible that the exposure that was sufficient in producing adaptations at the beginning of the acclimation period produces an insufficient thermal impulse at the later stages of acclimation.4 Individuals may opt to either increase exercise intensity or thermal load as acclimation progresses to ensure further adaptations. Maintaining exercise intensity via a set heart rate or core temperature provides an objective measure of adjustment, whereas increasing environmental temperature while using constant workload (e.g., watts on an ergometer bicycle or running pace) adjusts the thermal load while refraining from changes to exercise intensity. Flexibility to athlete’s heat acclimation strategy and training can be provided by using more than one protocol during the acclimation period.3 Nevertheless, it is important to be cautious at the beginning of the acclimation period when heat tolerance is still low. Hence, athletes should start acclimating with low intensity exercise and moderate heat. Intensity can be increased after the first three days of exposure as the initial adaptations have been made, reducing the risk of heat related illness, and increasing exercise-heat tolerance. Increasing intensity after the initial adaptations also increases sport specificity which is essential as peak performance in the heat is usually expected after the heat acclimation period.3
Acclimation Decay and Re-Acclimation
There are various reasons that can prevent an athlete from performing daily heat acclimation during the tapering period before an important competition thus forcing the athlete to acclimate in advance. Practical arrangements, structure of training, and personal preference should be considered when choosing the optimal protocol. As the adaptations from re-introduction to heat emerge considerably faster, the athlete may opt to perform a short heat re-acclimation period at the end of the taper to gain the full benefits of previous heat acclimation. Optionally, the athlete may choose to perform intermittent heat exposure in an effort to maintain adaptations.4 With intermittent heat exposure, acclimation decay can be attenuated by performing 1—2 heat exposures per week. However, even then a partial loss of adaptation can be seen, and a short re-acclimation is encouraged following a prolonged period of intermittent exposure.7 It is unclear how many weekly exposures would be sufficient in maintaining full adaptations and individual variability most likely exists. If using multiple exposures per week during intermittent heat exposure, passive methods may be preferred on occasion to maintain training quality during the taper.3 Similarly to training-related adaptations, the adaptations obtained from heat acclimation are eventually lost if exposure seizes. While considerable individual variability is present in the time span of acclimation decay, research suggests that on average a decrease of 35 % in heart rate, 30 % in sweat rate, and 6 % in core temperature adaptations can be expected during the first two weeks after an exposure ends.4
Heat acclimation is crucial to athletes, soldiers, workers, and fitness enthusiasts performing in hot environments to maximize physical performance and safety. Individuals can choose their preferred method of acclimation from a wide range of acclimation protocols including both active and passive methods. For best results, it is important to consider when peak performance is needed and whether intermittent heat exposure or heat re-acclimation is necessary. EP2 FINLAND brings the aid and assistance of field experts to your disposal. Utilizing these resources to guide you through heat acclimation can increase your chance of success.
References:
1. Périard, J., Eijsvogels, T., Daanen, H. 2021. Exercise Under Heat Stress: Thermoregulation, Hydration, Performance Implications, and Mitigation Strategies. Physiological Reviews 101, 1873—1979.
2. de Korte, J.Q., Bongers, C.C.W.G., Hopman, M.T.E., & Eijsvogels, T. M. H. 2021. Exercise Performance and Thermoregulatory Responses of Elite Athletes Exercising in the Heat: Outcomes of the Thermo Tokyo Study. Sports Medicine 51, 2423–2436. https://doi.org/10.1007/s40279-021-01530-w
3. Pryor, J., Johnson, E., Roberts, W., & Pryor, R. 2019. Application of evidence-based recommendations for heat acclimation: Individual and team sport perspectives. Temperature 6 (1), 37—49.
4. Daanen, H., Racinais, S., & Périard, J. 2017. Heat Acclimation Decay and Re-Induction: A Systematic Review and Meta-Analysis. Sports Medicine 48, 409—430.
5. Lundby, C., Svendsen, I., Urianstad, T., Hansen, J., & Rønnestad, B. 2021. Training Wearing Thermal Clothing and Training in Hot Ambient Conditions Are Equally Effective Methods of Heat Acclimation. Journal of Science and Medicine in Sport 24, 763—767.
6. Racinais, S., Périard, J.D., Alonso, J.M., Adami, P.E., & Bermon, S. 2019. Beat the Heat. IAAF World Athletics Championships Doha 2019 and the Tokyo 2020 Olympics.
7. Pryor, J.L., Pryor, R., Casa, D., Armstrong, L., Distefano, L., Anderson, J., Li, X., & Maresh, C. 2017. Effectiveness of an Intermittent Exercise-Heat Exposure Protocol to Sustain Heat Acclimation Adaptations. British Journal of Sports Medicine 51 (4). 375.2-375. 10.1136/bjsports-2016-097372.232.
Authors:
Jere Borgenström, MSc;
Juha Peltonen, PhD, Adjunct Professor
Christina Kuorelahti, PhD
Dominique Gagnon, PhD, Adjunct Professor
