Competing, training, and operating in cold environments present unique physiological challenges that athletes, coaches, and military personnel must navigate to achieve peak performance. Tissue cooling during cold exposure can alter neuromuscular function, decrease movement economy, and activate cold-defence mechanisms that preserve core temperature. By understanding these effects and implementing effective strategies exposed individuals can support physical performance and mitigate cold-induced detriments and hazards.
Acute Effects of Cold Exposure
Humans strive to maintain a core temperature of approximately 37 °C. During cold stress, heat loss may surpass heat production, leading to a drop in body temperature. The extent of this change is determined by the heat balance equation, which consists of heat exchange with the environment (radiation, convection, conduction, and evaporation) and metabolic heat production (physical activity, shivering, and non-shivering thermogenesis).
With decreasing body temperature, the human body activates cold-defence mechanisms to increase heat production and minimize heat loss. Peripheral vasoconstriction is the body’s first line of defence, reducing blood flow to the extremities to preserve core temperature. As blood circulation to the arms and legs decreases, their temperature drops, narrowing the temperature gradient between the skin and the surrounding environment. This process effectively decreases heat loss and helps to maintain core temperature in cold conditions.1 This is followed by the increase in heat production via shivering thermogenesis and non-shivering thermogenesis: the production of heat by involuntary muscle contractions and increasing metabolic activity. While shivering thermogenesis can increase metabolic rate up to fivefold, the increase in metabolic activity has a more modest effect.2
In addition to these involuntary cold-defence mechanisms, humans employ behavioural adjustments to generate heat. Individuals exposed to cold naturally increase physical activity, whether through exercise, fidgeting, or other spontaneous movement, to further boost metabolic heat production.1 For reference, intense exercise can raise metabolic rate 15- to 20-fold, making it the most effective way to generate heat in cold environments.2
Physical Performance in the Cold
When heat loss exceeds heat production, the body begins to cool down, leading to physiological impairments in cardiovascular function, energy delivery, nerve conduction speed, skeletal muscle contraction, and perception of effort, ultimately reducing both aerobic and anaerobic performance, and limiting strength, endurance, as well as coordination in cold environments.3
Endurance Performance
Endurance performance is noticeably influenced by environmental temperature, when temperatures shift away from a commonly considered temperate environment (~20 °C) toward hot or cold extremes. While a moderate decline in environmental temperature can actually enhance endurance performance by preventing the excessive increase in core temperature, a more drastic drop in temperature hinders it as oxygen consumption at a given work rate increases and time to exhaustion decreases.4,5
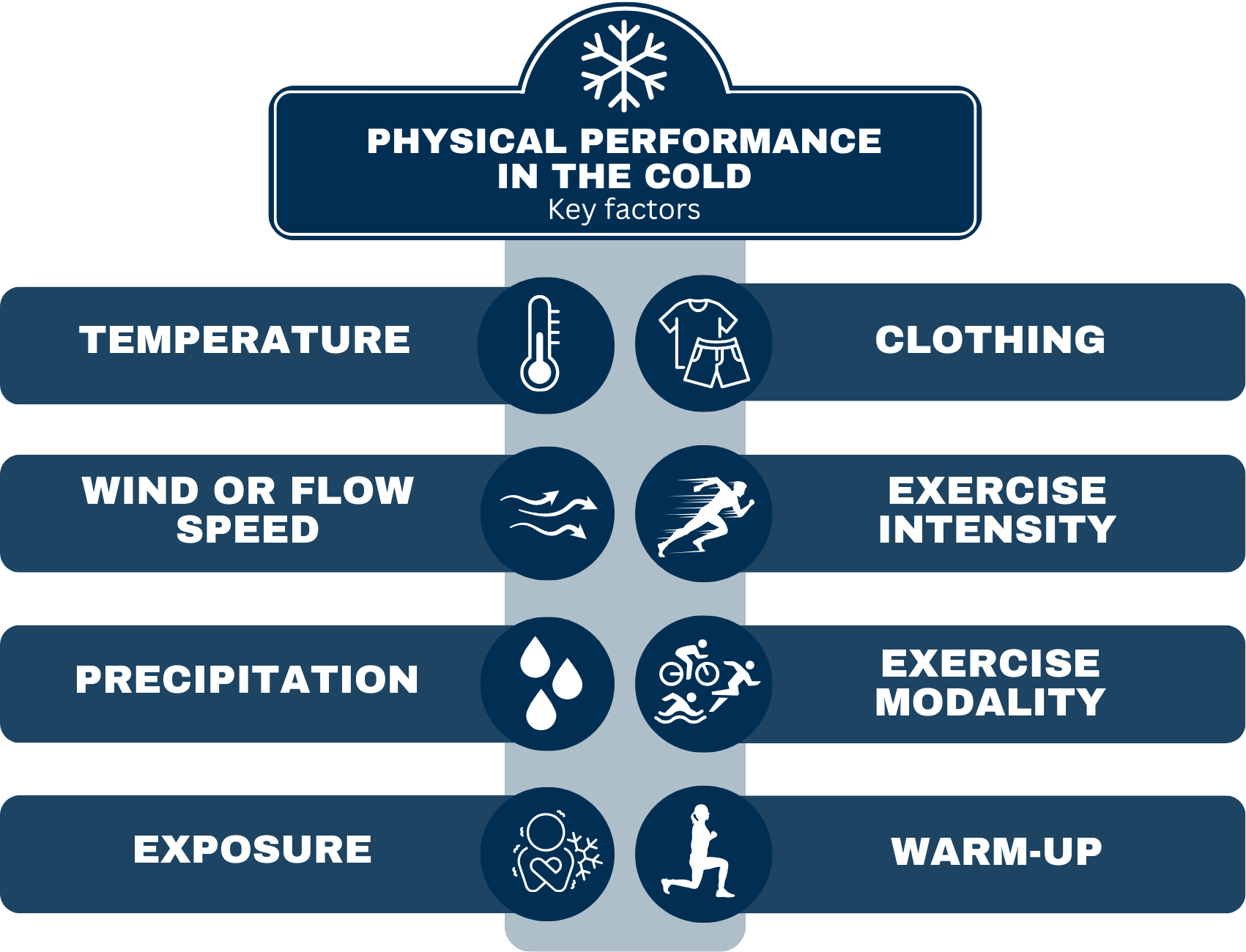
One contributing factor is the decline in movement economy when muscles are cooled. This increases submaximal oxygen consumption, placing greater metabolic demand and need for oxygen on the body, ultimately limiting endurance capacity.⁸ Maintaining heat with extra clothing poses its own challenges, as each additional kilogram of clothing increases energy cost by ~3 % and each additional layer by ~4 %.⁹ Finding the right balance between insulation and mobility is crucial for sustaining endurance performance in cold conditions. Laboratory research suggests that individuals wearing shorts and t-shirts can achieve optimal endurance performance at around 10 °C4, while those dressed in a light skiing suit with long-sleeved undergarments performed best at -4 °C.5 Thus it is clear that temperature alone does not dictate performance outcomes — clothing, exercise intensity, modality, and additional environmental factors such as wind speed, humidity, and precipitation all play a critical role in shaping physiological responses, thermal balance, and overall performance in cold conditions.
Endurance athletes should stay warm enough to maintain movement efficiency while preventing excessive increase in core temperature. Higher-intensity exercise generates more heat, allowing for lighter clothing, whereas lower-intensity efforts require additional insulation to maintain thermal balance. When temperatures are low, staying in warm indoor conditions and minimizing exposure before exercise helps prevent unnecessary muscle cooling, which would otherwise reduce efficiency and increase energy demands10. If avoiding exposure is not possible, external heating methods – such as insulative or heated clothing and warming packs – can be used to maintain muscle temperature before exercise begins. Additionally, a structured and extended warm-up period can play a crucial role in counteracting the negative effects of cold exposure and preparing the body for peak performance10.
Strength, Power, and Coordination
The effect of environmental temperature on muscle force and power production is well-documented: exposure to cool and cold environments lowers tissue temperature, leading to decreased muscle force output. Even a modest drop in muscle temperature – whether systemic or localized – can negatively impact strength and power.3 To compensate for the impaired mechanical and contractile properties of muscles, the body recruits more muscle fibers to perform the same amount of work, increasing energy expenditure and reducing efficiency. Efficiency is further reduced by the increased co-activation of agonist and antagonist muscle pairs, where both the recruited muscle and the one creating an opposing force will be activated. Cold muscle tissue is also characterized by a leftward shift in the force-velocity curve: less force can be produced at a given contraction velocity, thereby reducing power.3 Beyond strength and power, coordination and balance also decline in the cold, increasing both performance limitations and injury risk.³ To maximize performance and safety in strength and power sports, maintaining muscle heat through proper warm-ups, passive heating, and insulative clothing should be a key focus when competing in cool or cold conditions.
Cold-Related Injuries
The decline in physical performance is not the only concern in cold environments – cold-related injuries, ranging from mild frostbite to life-threatening hypothermia, pose significant risks. Proper preparation is essential to manage these hazards and to ensure safety during cold exposure. With appropriate clothing, suitable equipment, and the right knowledge, cold exposure can be done safely. However, it is important to recognize that individual responses to cold vary, and even with identical clothing and gear, some individuals may be more susceptible to cold-related injuries than others7. Especially children and the elderly as well as those suffering from vascular dysfunctions may be susceptible to cold-related injuries.
Frostbite is the most common health hazard for athletes and soldiers during cold exposure, occurring when skin temperature drops below -0.5°C, causing tissue to freeze. Fingers, toes, nose, and ears are particularly vulnerable, as they are far from the body’s core and highly affected by cold-induced vasoconstriction, which reduces blood flow and heat supply. The primary causes of frostbite include inadequate clothing and equipment, as well as a lack of knowledge about cold exposure.6 An additional risk is contact cooling, which occurs when gripping highly conductive materials such as metal in cold environments, accelerating heat loss and increasing frostbite risk.7 Warming of the affected area should be done when the risk of refreezing is minimised, as refreezing can further contribute to the injury. Using warm water (~37 °C) is recommended for the rewarming process.6
Hypothermia is defined as the decrease in core temperature below 35,0 °C, and it can be categorized as mild (35—32 °C), moderate (32—28 °C) or severe (< 28 °C). Mild hypothermia is characterized by intensive shivering, social withdrawal, and other behavioural changes. During moderate hypothermia shivering decreases and finally stops entirely and the individual becomes confused or loses consciousness. A risk of arrythmias is present. Finally, when reaching severe hypothermia heart arrythmias and death become more likely.6 Early recognition and preparation are key to preventing hypothermia. If hypothermia occurs, mild cases can be managed by passive rewarming—allowing the body to generate heat through shivering in a warm, dry environment. More severe cases may require active heating strategies, but caution is necessary, as sudden movements can trigger arrhythmias, and rapid rewarming may worsen the situation in moderately and severely hypothermic individuals.6 While reaching hypothermia during intense exercise is unlikely in most situations, events with significantly increased heat loss, such as open-water swimming, pose a high risk for participants11. The risk for hypothermia can be increased in land-based sports as well, especially when low temperatures are combined with rain, high movement or wind speeds, and prolonged exposure.
Cold Acclimation
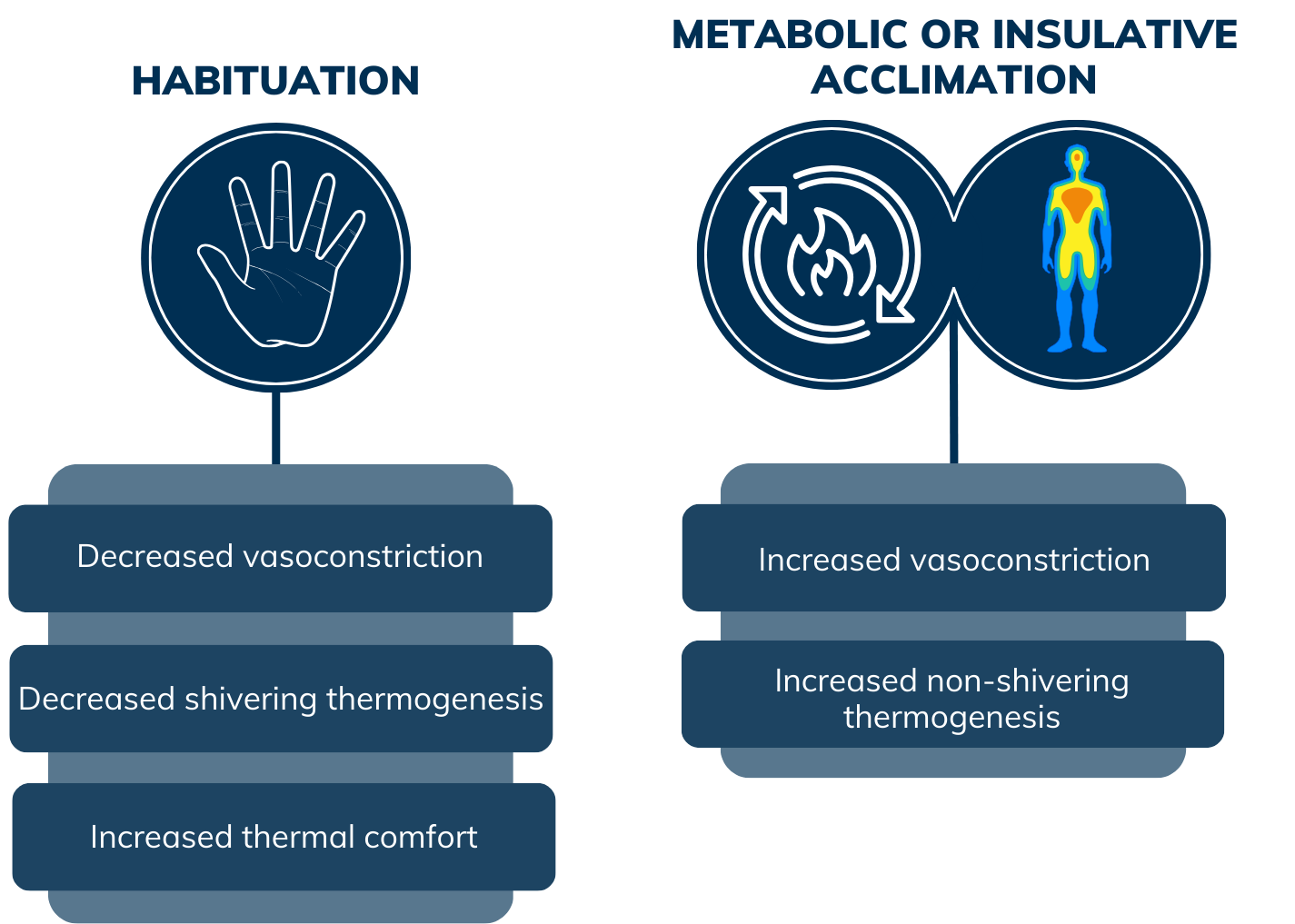
The body’s adaptation to prolonged cold exposure is not entirely clear, but research has identified three distinct acclimation responses: habituation, metabolic adaptation, and insulative adaptation. Habituation is the most common response, where shivering and vasoconstriction responses become blunted after repeated cold exposure. This reduces discomfort and increases tolerance to cold, but it also allows for a faster drop in core temperature due to increased heat loss and reduced heat production. Metabolic adaptation involves an increased metabolic response, particularly through enhanced non-shivering thermogenesis (NST) to generate more heat. Insulative adaptation refers to an increased vasoconstrictive response, which further reduces blood flow to the extremities to minimize heat loss and better preserve core temperature. The type of acclimation response may depend on the extent of deep body heat loss and whether the cold stress is metabolically compensable – meaning if shivering and non-shivering thermogenesis can adequately defend core temperature. However, metabolic and insulative adaptations are generally small and may not play a major role in long-term survival and success in cold conditions.1 A daily one-hour exposure to cold-water (14 C°) immersion for seven consecutive days has been shown to be enough to elicit reduced shivering and increased NST.12 Research on cold acclimation’s effect on physical performance is limited, and there is no strong evidence to suggest that any form of cold acclimation significantly enhances physical performance in cold environments.
Cold environments present unique challenges for athletes, coaches, and military personnel, impacting physical performance, injury risk, and overall physiological function. Though cold acclimation may improve comfort and tolerance, its impact on performance remains unclear. However, with proper clothing, training, and knowledge individuals can minimize cold-related risks and maintain performance in extreme conditions. EP2 FINLAND brings the aid and assistance of field experts to your disposal. Utilizing these resources to guide you through cold exposure can increase your chance of success.
References:
1. Castellani, J. & Young, A. 2016. Human physiological responses to cold exposure: Acute responses and acclimatization to prolonged exposure. Autonomic Neuroscience: Basic and Clinical 196, 63—74.
2. Haman, F. & Blondin, D. 2017. Shivering thermogenesis in humans: origin, contribution and metabolic requirement. Temperature 4(3), 217—226.
3. Castellani, J. & Tipton, M. 2015. Cold Stress Effects on Exposure Tolerance and Exercise Performance. Comprehensive Physiology 6, 443—469.
4. Galloway, S. & Maughan, R. 1997. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Medicine and Science in Sport and Exercise 29(9), 1240—9.
5. Sandsund, M., Saursaunet, V., Wiggen, Ø., Renberg, J., Færevik, H., & van Beekvelt, M. C. P. 2012. Effect of ambient temperature on endurance performance while wearing cross-country skiing clothing. European Journal of Applied Physiology, 112(12), 3939–3947.
6. Fudge, J. Exercise in the Cold: Preventing and Managing Hypothermia and Frostbite Injury. Sports Health 8(2), 133—139.
7. Haman, F., Souza, S. C. S., Castellani, J. W., Dupuis, M. P., Friedl, K. E., Sullivan-Kwantes, W., & Kingma, B. R. M. 2022. Human vulnerability and variability in the cold: Establishing individual risks for cold weather injuries. Temperature 9(2), 158–195.
8. Oksa, J., Kaikkonen, H., Sorvisto, P., Vaappo, M., Martikkala, V., & Rintamäki, H. 2004. Changes in maximal cardiorespiratory capacity and submaximal strain while exercising in cold. Journal of Thermal Biology 29(7-8), 815–818.
9. Rintamäki, H. 2007. Performance and energy expenditure in cold environments. Alaska medicine, 49(2), 245–246.
10. Kruk, B., Pekkarinen, H., Harri, M., Manninen, K., & Hanninen, O. 1990. Thermoregulatory responses to exercise at low ambient temperature performed after precooling or preheating procedures. European Journal of Applied Physiology and Occupational Physiology 59(6), 416–420.
11. Brannigan, D., Rogers, I. R., Jacobs, I., Montgomery, A., Williams, A., & Khangure, N. 2009. Hypothermia Is a Significant Medical Risk of Mass Participation Long-Distance Open Water Swimming. Wilderness & Environmental Medicine, 20(1), 14–18.
12. Gordon K, Blondin DP, Friesen BJ, Tingelstad HC, Kenny GP, Haman F. 2019. Seven days of cold acclimation substantially reduces shivering intensity and increases nonshivering thermogenesis in adult humans. Journal of Applied Physiology 126(6), 1598-1606.
13. Gatterer, H., Dünnwald, T., Turner, R., Csapo, R., Schobersberger, W., Burtscher, M., Faulhaber, M., & Kennedy, M. D. (2021). Practicing Sport in Cold Environments: Practical Recommendations to Improve Sport Performance and Reduce Negative Health Outcomes. International Journal of Environmental Research and Public Health, 18(18), 9700.
Authors:
Jere Borgenström, MSc;
Juha Peltonen, PhD, Adjunct Professor
Dominique Gagnon, PhD, Adjunct Professor
